Esophageal Cancer Treatment (PDQ®): Treatment - Health Professional Information [NCI]
Esophageal Cancer Treatment (PDQ®): Treatment - Health Professional Information [NCI]Skip to the navigationGeneral Information About Esophageal CancerTwo histologic types account for the majority of malignant esophageal neoplasms: adenocarcinoma and squamous carcinoma. Adenocarcinomas typically start in the lower esophagus and squamous cell carcinoma can develop throughout the esophagus. The epidemiology of these types varies markedly. Incidence and Mortality Estimated new cases and deaths from esophageal cancer in the United States in 2017:[1] - New cases: 16,940.
- Deaths: 15,690.
The incidence of esophageal cancer has risen in recent decades, coinciding with a shift in histologic type and primary tumor location. In the United States, squamous cell carcinoma has historically been more prevalent although the incidence of adenocarcinoma has risen dramatically in the last few decades in the United States and western Europe.[2,3] Worldwide, squamous cell carcinoma remains the predominant histology, however, adenocarcinoma of the esophagus is now more prevalent than squamous cell carcinoma in the United States and western Europe.[4] The incidence of adenocarcinoma has increased most notably among white males.[5] In the United States, the median age of patients who present with esophageal cancer is 67 years.[6] The majority of adenocarcinomas are located in the distal esophagus. The cause for the rising incidence and demographic alterations is unknown. Anatomy
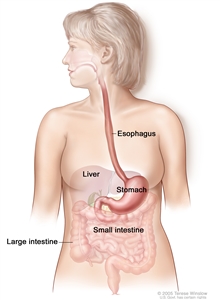
The esophagus and stomach are part of the upper gastrointestinal (digestive) system.
The esophagus serves as a conduit to the gastrointestinal tract for food. The esophagus extends from the larynx to the stomach and lies in the posterior mediastinum within the thorax in close proximity to the lung pleura, peritoneum, pericardium, and diaphragm. As it travels into the abdominal cavity, the esophagus makes an abrupt turn and enters the stomach. The esophagus is the most muscular segment of the gastrointestinal system and is composed of inner circular and outer longitudinal muscle layers. The upper and lower esophagus are controlled by the sphincter function of the cricopharyngeus muscle and gastroesophageal sphincter, respectively. The esophagus has a rich network of lymphatic channels concentrated in the lamina propria and submucosa, which drains longitudinally along the submucosa. Tumors of the esophagus are conventionally described in terms of distance of the upper border of the tumor to the incisors. When measured from the incisors via endoscopy, the esophagus extends approximately 30 to 40 cm. The esophagus is divided into four main segments: - Cervical esophagus (~15-20 cm from the incisors).
- Upper thoracic esophagus (~20-25 cm from the incisors).
- Middle thoracic esophagus (~25-30 cm from the incisors).
- Lower thoracic esophagus and gastroesophageal junction (~30-40 cm from the incisors).
Risk Factors Risk factors for squamous cell carcinoma of the esophagus include: Risk factors associated with esophageal adenocarcinoma are less clear.[3] Barrett esophagus is an exception and its presence is associated with an increased risk of developing adenocarcinoma of the esophagus. Chronic reflux is considered the predominant cause of Barrett metaplasia. The results of a population-based, case-controlled study from Sweden strongly suggest that symptomatic gastroesophageal reflux is a risk factor for esophageal adenocarcinoma. The frequency, severity, and duration of reflux symptoms were positively correlated with increased risk of esophageal adenocarcinoma.[7] (Refer to the PDQ summary on Esophageal Cancer Prevention for more information.) Prognostic Factors Favorable prognostic factors include the following: - Early-stage disease.
- Complete resection.
Patients with severe dysplasia in distal esophageal Barrett mucosa often have in situ or invasive cancer within the dysplastic area. After resection, these patients usually have excellent prognoses.[8] In most cases, esophageal cancer is a treatable disease, but it is rarely curable. The overall 5-year survival rate in patients amenable to definitive treatment ranges from 5% to 30%. The occasional patient with very early disease has a better chance of survival. Related Summaries Other PDQ summaries containing information related to esophageal cancer include the following: - Esophageal Cancer Prevention
- Esophageal Cancer Screening
- Unusual Cancers of Childhood Treatment
For information about gastrointestinal stromal tumors, which can occur in the esophagus and are usually benign, refer to the following summary: - Gastrointestinal Stromal Tumors Treatment
For information about supportive care for patients with esophageal cancer, refer to the following summaries: - Nutrition in Cancer Care
- Dysphagia section in the Oral Complications of Chemotherapy and Head/Neck Radiation summary
References:
-
American Cancer Society: Cancer Facts and Figures 2017. Atlanta, Ga: American Cancer Society, 2017. Available online. Last accessed May 25, 2017.
-
Brown LM, Devesa SS, Chow WH: Incidence of adenocarcinoma of the esophagus among white Americans by sex, stage, and age. J Natl Cancer Inst 100 (16): 1184-7, 2008.
-
Blot WJ, McLaughlin JK: The changing epidemiology of esophageal cancer. Semin Oncol 26 (5 Suppl 15): 2-8, 1999.
-
Schmassmann A, Oldendorf MG, Gebbers JO: Changing incidence of gastric and oesophageal cancer subtypes in central Switzerland between 1982 and 2007. Eur J Epidemiol 24 (10): 603-9, 2009.
-
Kubo A, Corley DA: Marked multi-ethnic variation of esophageal and gastric cardia carcinomas within the United States. Am J Gastroenterol 99 (4): 582-8, 2004.
-
Ginsberg RJ: Cancer treatment in the elderly. J Am Coll Surg 187 (4): 427-8, 1998.
-
Lagergren J, Bergström R, Lindgren A, et al.: Symptomatic gastroesophageal reflux as a risk factor for esophageal adenocarcinoma. N Engl J Med 340 (11): 825-31, 1999.
-
Reed MF, Tolis G Jr, Edil BH, et al.: Surgical treatment of esophageal high-grade dysplasia. Ann Thorac Surg 79 (4): 1110-5; discussion 1110-5, 2005.
Cellular Classification of Esophageal CancerAdenocarcinomas, typically arising in Barrett esophagus, account for at least 50% of malignant lesions, and the incidence of this histology appears to be rising. Barrett esophagus contains glandular epithelium cephalad to the esophagogastric junction. Three different types of glandular epithelium can be seen: - Metaplastic columnar epithelium.
- Metaplastic parietal cell glandular epithelium within the esophageal wall.
- Metaplastic intestinal epithelium with typical goblet cells. Dysplasia is particularly likely to develop in the intestinal type mucosa.
Fewer than 50% of esophageal cancers are squamous cell carcinomas. Gastrointestinal stromal tumors can occur in the esophagus and are usually benign. (Refer to the PDQ summary on Gastrointestinal Stromal Tumors Treatment for more information.) Stage Information for Esophageal CancerOne of the major difficulties in allocating and comparing treatment modalities for patients with esophageal cancer is the lack of precise preoperative staging. The stage determines whether the intent of the therapeutic approach will be curative or palliative. Staging Evaluation Standard noninvasive staging modalities include the following: - Endoscopic ultrasound.
- Computed tomography (CT) scan of the chest and abdomen.
- Positron emission tomography (PET)-CT scan.
The overall tumor depth staging accuracy of endoscopic ultrasound is 85% to 90%, compared with 50% to 80% for CT; the accuracy of regional nodal staging is 70% to 80% for endoscopic ultrasound and 50% to 70% for CT.[1,2] One retrospective series reported a 93% sensitivity and 100% specificity of regional nodal staging with endoscopic ultrasound-guided fine-needle aspiration (FNA). Endoscopic ultrasound-guided FNA for lymph node staging is under prospective evaluation.[3] Thoracoscopy and laparoscopy have been used in esophageal cancer staging at some surgical centers.[4,5,6] An intergroup trial reported an increase in positive lymph node detection to 56% of 107 evaluable patients with the use of thoracoscopy/laparoscopy, from 41% (with the use of noninvasive staging tests, e.g., CT, magnetic resonance imaging, and endoscopic ultrasound), with no major complications or deaths.[7] Noninvasive PET scan using the radiolabeled glucose analog 18-F-fluorodeoxy-D-glucose (FDG) for preoperative staging of esophageal cancer is more sensitive than a CT scan or endoscopic ultrasound in detection of distant metastases. A recent study of 262 patients with potentially resectable esophageal cancer demonstrated the utility of FDG-PET in identifying confirmed distant metastatic disease in at least 4.8% of patients after standard evaluation.[8,9,10,11,12] AJCC Staging System The American Joint Committee on Cancer (AJCC) has designated staging by TNM classification to define cancer of the esophagus and esophagogastric junction.[13] Tumors located in the gastric cardia within 5 cm of the gastroesophageal junction with extension into the esophagus or the gastroesophageal junction are classified as esophageal cancer. Tumors with the epicenter of the tumor located in the gastric cardia beyond 5 cm of the gastroesophageal junction or without extension into the esophagus are classified as gastric cancer.[13] (Refer to the Stage Information section in the PDQ summary on Gastric Cancer Treatment for more information.) In contrast to earlier classification systems, the 2010 AJCC TNM staging system differentiates by histologic subtype, with an individualized staging system for squamous cell carcinoma versus adenocarcinoma, reflecting differences in inherent biology.[13] The classification of involved abdominal lymph nodes as M1 disease is controversial. The presence of positive abdominal lymph nodes does not appear to have a prognosis as grave as that for metastases to distant organs.[14] Patients with regional and/or celiac axis lymphadenopathy should not necessarily be considered to have unresectable disease caused by metastases. Complete resection of the primary tumor and appropriate lymphadenectomy should be attempted when possible. Staging for squamous cell carcinoma of the esophagus Table 1. Definitions of TNM Stage 0 Squamous Cell Carcinoma| Stage | Grade | Tumor Locationa | TNMb,c | Description |
|---|
| T = primary tumor; N = regional lymph nodes; M = distant metastasis. | | Reprinted with permission from AJCC: Esophageal and esophagogastric junction. In: Edge SB, Byrd DR, Compton CC, et al., eds.: AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer, 2010, pp 103-15. | | The explanations for superscripts a-d are at the end of Table 9. | | 0 | 1, X | Any | Tis, N0, M0 | Tis = High-grade dysplasia.d | | N0 = No regional lymph node metastasis. | | M0 = No distant metastasis. | Table 2. Definitions of TNM Stage IA Squamous Cell Carcinoma| Stage | Grade | Tumor Locationa | TNMb,c | Description | Illustration |
|---|
| T = primary tumor; N = regional lymph nodes; M = distant metastasis. | | Reprinted with permission from AJCC: Esophageal and esophagogastric junction. In: Edge SB, Byrd DR, Compton CC, et al., eds.: AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer, 2010, pp 103-15. | | The explanations for superscripts a-c are at the end of Table 9. | | IA | 1, X | Any | T1, N0, M0 | T1 = Tumor invades lamina propria, muscularis mucosae, or submucosa. |
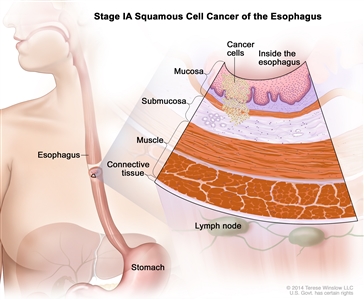
Stage IA squamous cell cancer of the esophagus. Cancer has formed in the mucosa or submucosa layer of the esophagus wall. The cancer cells are grade 1 or the grade is unknown. Grade 1 cancer cells look more like normal cells under a microscope and grow and spread more slowly than grade 2-3 cancer cells. | | N0 = No regional lymph node metastasis. | | M0 = No distant metastasis. | Table 3. Definitions of TNM Stage IB Squamous Cell Carcinoma| Stage | Grade | Tumor Locationa | TNMb,c | Description | Illustration |
|---|
| T = primary tumor; N = regional lymph nodes; M = distant metastasis. | | Reprinted with permission from AJCC: Esophageal and esophagogastric junction. In: Edge SB, Byrd DR, Compton CC, et al., eds.: AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer, 2010, pp 103-15. | | The explanations for superscripts a-c are at the end of Table 9. | | IB | 2-3 | Any | T1, N0, M0 | T1 = Tumor invades lamina propria, muscularis mucosae, or submucosa. |
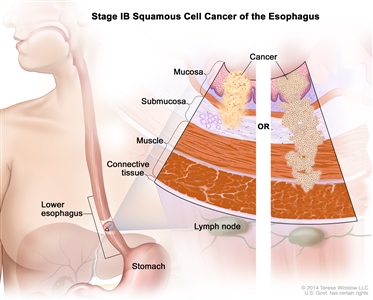
Stage IB squamous cell cancer of the esophagus. Cancer has formed in the mucosa or submucosa layer of the esophagus wall, and the cancer cells are grade 2-3; OR cancer has formed in the mucosa or submucosa layer and spread into the muscle layer or the connective tissue layer of the esophagus wall, and the cancer cells are grade 1. Grade 1 cancer cells look more like normal cells under a microscope and grow and spread more slowly than grade 2-3 cancer cells. The tumor is in the lower esophagus or it is not known where the tumor is. | | N0 = No regional lymph node metastasis. | | M0 = No distant metastasis. | | 1, X | Lower, X | T2-3, N0, M0 | T2 = Tumor invades muscularis propria. | | T3 = Tumor invades adventitia. | | N0 = No regional lymph node metastasis. | | M0 = No distant metastasis. | Table 4. Definitions of TNM Stage IIA Squamous Cell Carcinoma| Stage | Grade | Tumor Locationa | TNMb,c | Description | Illustration |
|---|
| T = primary tumor; N = regional lymph nodes; M = distant metastasis. | | Reprinted with permission from AJCC: Esophageal and esophagogastric junction. In: Edge SB, Byrd DR, Compton CC, et al., eds.: AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer, 2010, pp 103-15. | | The explanations for superscripts a-c are at the end of Table 9. | | IIA | 1, X | Upper, middle | T2-3, N0, M0 | T2 = Tumor invades muscularis propria. |
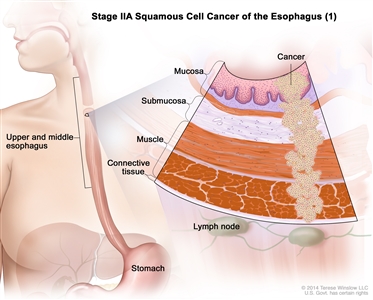
Stage IIA squamous cell cancer of the esophagus (1). The tumor is in either the upper or middle esophagus. Cancer has spread into the muscle layer or the connective tissue layer of the esophagus wall. The cancer cells are grade 1. Grade 1 cancer cells look more like normal cells under a microscope and grow and spread more slowly than grade 2-3 cancer cells.
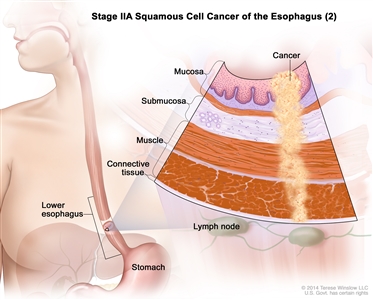
Stage IIA squamous cell cancer of the esophagus (2). The tumor is in the lower esophagus or it is not known where the tumor is. Cancer has spread into the muscle layer or the connective tissue layer of the esophagus wall. The cancer cells are grade 2-3. Grade 2-3 cancer cells look more abnormal under a microscope and grow and spread more quickly than grade 1 cancer cells. | | T3 = Tumor invades adventitia. | | N0 = No regional lymph node metastasis. | | M0 = No distant metastasis. | | 2-3 | Lower, X | T2-3, N0, M0 | T2 = Tumor invades muscularis propria. | | T3 = Tumor invades adventitia. | | N0 = No regional lymph node metastasis. | | M0 = No distant metastasis. | Table 5. Definitions of TNM Stage IIB Squamous Cell Carcinoma| Stage | Grade | Tumor Locationa | TNMb,c | Description | Illustration |
|---|
| T = primary tumor; N = regional lymph nodes; M = distant metastasis. | | Reprinted with permission from AJCC: Esophageal and esophagogastric junction. In: Edge SB, Byrd DR, Compton CC, et al., eds.: AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer, 2010, pp 103-15. | | The explanations for superscripts a-c are at the end of Table 9. | | IIB | 2-3 | Upper, middle | T2-3, N0, M0 | T2 = Tumor invades muscularis propria. |
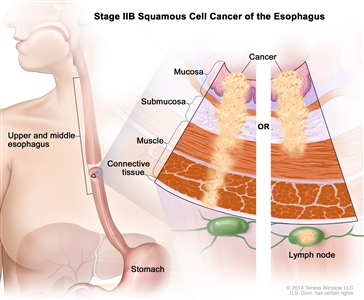
Stage IIB squamous cell cancer of the esophagus. The tumor is in either the upper or middle esophagus. Cancer has spread into the muscle layer or the connective tissue layer of the esophagus wall, and the cancer cells are grade 2-3; OR cancer is in the mucosa or submucosa layer and may have spread into the muscle layer of the esophagus wall, and cancer is found in 1 or 2 lymph nodes near the tumor. Grade 2-3 cancer cells look more abnormal under a microscope and grow and spread more quickly than grade 1 cancer cells. | | T3 = Tumor invades adventitia. | | N0 = No regional lymph node metastasis. | | M0 = No distant metastasis. | | Any | Any | T1-2, N1, M0 | T1 = Tumor invades lamina propria, muscularis mucosae, or submucosa. | | T2 = Tumor invades muscularis propria. | | N1 = Metastases in 1-2 regional lymph nodes. | | M0 = No distant metastasis. | Table 6. Definitions of TNM Stage IIIA Squamous Cell Carcinoma| Stage | Grade | Tumor Locationa | TNMb,c | Description | Illustration |
|---|
| T = primary tumor; N = regional lymph nodes; M = distant metastasis. | | Reprinted with permission from AJCC: Esophageal and esophagogastric junction. In: Edge SB, Byrd DR, Compton CC, et al., eds.: AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer, 2010, pp 103-15. | | The explanations for superscripts a-c are at the end of Table 9. | | IIIA | Any | Any | T1-2, N2, M0 | T1 = Tumor invades lamina propria, muscularis mucosae, or submucosa. |
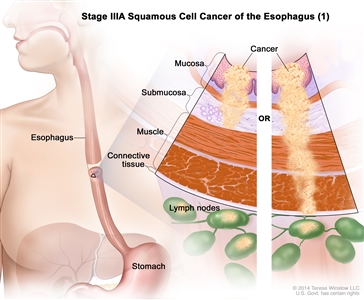
Stage IIIA squamous cell cancer of the esophagus (1). Cancer is in the mucosa or submucosa layer and may have spread into the muscle layer of the esophagus wall, and cancer is found in 3 to 6 lymph nodes near the tumor; OR cancer has spread into the connective tissue layer of the esophagus wall, and cancer is found in 1 or 2 lymph nodes near the tumor.
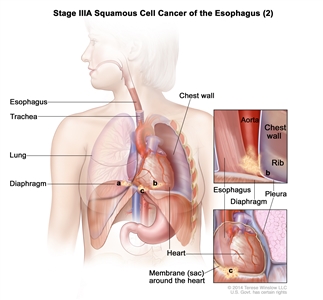
Stage IIIA squamous cell cancer of the esophagus (2). Cancer has spread into the (a) diaphragm, (b) pleura (tissue that covers the lungs and lines the inner wall of the chest cavity), or (c) membrane (sac) around the heart. The cancer can be removed by surgery. | | T2 = Tumor invades muscularis propria. | | N2 = Metastases in 3-6 regional lymph nodes. | | M0 = No distant metastasis. | | Any | Any | T3, N1, M0 | T3 = Tumor invades adventitia. | | N1 = Metastases in 1-2 regional lymph nodes. | | M0 = No distant metastasis. | | Any | Any | T4a, N0, M0 | T4a = Resectable tumor invading pleura, pericardium, or diaphragm. | | N0 = No regional lymph node metastasis. | | M0 = No distant metastasis. | Table 7. Definitions of TNM Stage IIIB Squamous Cell Carcinoma| Stage | Grade | Tumor Locationa | TNMb,c | Description | Illustration |
|---|
| T = primary tumor; N = regional lymph nodes; M = distant metastasis. | | Reprinted with permission from AJCC: Esophageal and esophagogastric junction. In: Edge SB, Byrd DR, Compton CC, et al., eds.: AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer, 2010, pp 103-15. | | The explanations for superscripts a-c are at the end of Table 9. | | IIIB | Any | Any | T3, N2, M0 | T3 = Tumor invades adventitia. |
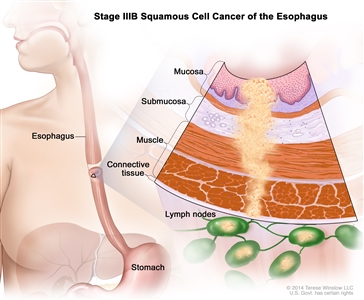
Stage IIIB squamous cell cancer of the esophagus. Cancer has spread into the connective tissue layer of the esophagus wall. Cancer is found in 3 to 6 lymph nodes near the tumor. | | N2 = Metastases in 3-6 regional lymph nodes. | | M0 = No distant metastasis. | Table 8. Definitions of TNM Stage IIIC Squamous Cell Carcinoma| Stage | Grade | Tumor Locationa | TNMb,c | Description | Illustration |
|---|
| T = primary tumor; N = regional lymph nodes; M = distant metastasis. | | Reprinted with permission from AJCC: Esophageal and esophagogastric junction. In: Edge SB, Byrd DR, Compton CC, et al., eds.: AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer, 2010, pp 103-15. | | The explanations for superscripts a-d are at the end of Table 9. | | IIIC | Any | Any | T4a, N1-2, M0 | T4a = Resectable tumor invading pleura, pericardium, or diaphragm. |
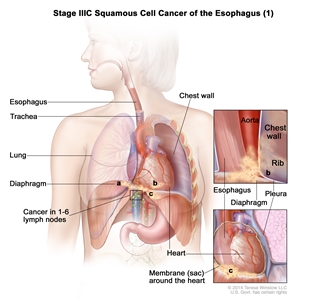
Stage IIIC squamous cell cancer of the esophagus (1). Cancer has spread into the (a) diaphragm, (b) pleura (tissue that covers the lungs and lines the inner wall of the chest cavity), or (c) membrane (sac) around the heart. The cancer can be removed by surgery. Cancer is found in 1 to 6 lymph nodes near the tumor.
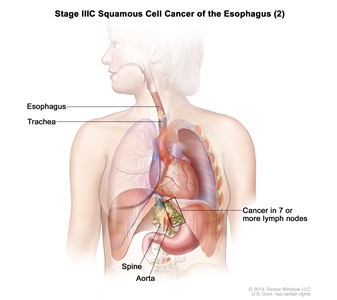
Stage IIIC squamous cell cancer of the esophagus (2). Cancer has spread into nearby organs, such as the aorta, trachea, or spine, and the cancer cannot be removed by surgery; OR cancer has spread to 7 or more lymph nodes near the tumor. | | N1 = Metastases in 1-2 regional lymph nodes. | | N2 = Metastases in 3-6 regional lymph nodes. | | M0 = No distant metastasis. | | Any | Any | T4b, Any N, M0 | T4b = Unresectable tumor invading other adjacent structures, such as aorta, vertebral body, trachea, etc. | | NX = Regional lymph nodes cannot be assessed. | | N0 = No regional lymph node metastasis. | | N1 = Metastases in 1-2 regional lymph nodes. | | N2 = Metastases in 3-6 regional lymph nodes. | | N3 = Metastases in ≥7 regional lymph nodes. | | M0 = No distant metastasis. | | Any | Any | Any T, N3, M0 | TX = Primary tumor cannot be assessed. | | T0 = No evidence of primary tumor. | | Tis = High-grade dysplasia.d | | T1 = Tumor invades lamina propria, muscularis mucosae, or submucosa. | | T1a = Tumor invades lamina propria or muscularis mucosae. | | T1b = Tumor invades submucosa. | | T2 = Tumor invades muscularis propria. | | T3 = Tumor invades adventitia. | | T4 = Tumor invades adjacent structures. | | T4a = Resectable tumor invading pleura, pericardium, or diaphragm. | | T4b = Unresectable tumor invading other adjacent structures, such as aorta, vertebral body, trachea, etc. | | N3 = Metastases in ≥7 regional lymph nodes. | | M0 = No distant metastasis. | Table 9. Definitions of TNM Stage IV Squamous Cell Carcinoma| Stage | Grade | Tumor Locationa | TNMb,c | Description | Illustration |
|---|
| T = primary tumor; N = regional lymph nodes; M = distant metastasis. | | Reprinted with permission from AJCC: Esophageal and esophagogastric junction. In: Edge SB, Byrd DR, Compton CC, et al., eds.: AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer, 2010, pp 103-15. | | a Location of the primary cancer site is defined by the position of the upper (proximal) edge of the tumor in the esophagus. | | b(1) At least maximal dimension of the tumor must be recorded, and (2) multiple tumors require the T(m) suffix. | | c Number must be recorded for total number of regional nodes sampled and total number of reported nodes with metastasis. | | d High-grade dysplasia includes all noninvasive neoplastic epithelia that was formerly called carcinoma in situ, a diagnosis that is no longer used for columnar mucosae anywhere in the gastrointestinal tract. | | IV | Any | Any | Any T, Any N, M1 | TX = Primary tumor cannot be assessed. |
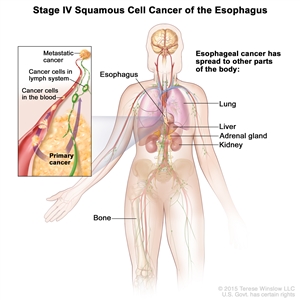
Stage IV squamous cell cancer of the esophagus. The cancer has spread to other parts of the body, such as the lung, liver, adrenal gland, kidney, or bone. | | T0 = No evidence of primary tumor. | | Tis = High-grade dysplasia.d | | T1 = Tumor invades lamina propria, muscularis mucosae, or submucosa. | | T1a = Tumor invades lamina propria or muscularis mucosae. | | T1b = Tumor invades submucosa. | | T2 = Tumor invades muscularis propria. | | T3 = Tumor invades adventitia. | | T4 = Tumor invades adjacent structures. | | T4a = Resectable tumor invading pleura, pericardium, or diaphragm. | | T4b = Unresectable tumor invading other adjacent structures, such as aorta, vertebral body, trachea, etc. | | NX = Regional lymph nodes cannot be assessed. | | N0 = No regional lymph node metastasis. | | N1 = Metastases in 1-2 regional lymph nodes. | | N2 = Metastases in 3-6 regional lymph nodes. | | N3 = Metastases in ≥7 regional lymph nodes. | | M1 = Distant metastasis. | Staging for adenocarcinoma of the esophagus Table 10. Definitions of TNM Stage 0 Adenocarcinoma| Stage | Grade | TNMa,b | Description |
|---|
| T = primary tumor; N = regional lymph nodes; M = distant metastasis. | | Reprinted with permission from AJCC: Esophageal and esophagogastric junction. In: Edge SB, Byrd DR, Compton CC, et al., eds.: AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer, 2010, pp 103-15. | | The explanations for superscripts a-c are at the end of Table 18. | | 0 | 1, X | Tis, N0, M0 | Tis = High-grade dysplasia.c | | N0 = No regional lymph node metastasis. | | M0 = No distant metastasis. | Table 11. Definitions of TNM Stage IA Adenocarcinoma| Stage | Grade | TNMa,b | Description | Illustration |
|---|
| T = primary tumor; N = regional lymph nodes; M = distant metastasis. | | Reprinted with permission from AJCC: Esophageal and esophagogastric junction. In: Edge SB, Byrd DR, Compton CC, et al., eds.: AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer, 2010, pp 103-15. | | The explanations for superscripts a-b are at the end of Table 18. | | IA | 1-2, X | T1, N0, M0 | T1 = Tumor invades lamina propria, muscularis mucosae, or submucosa. |
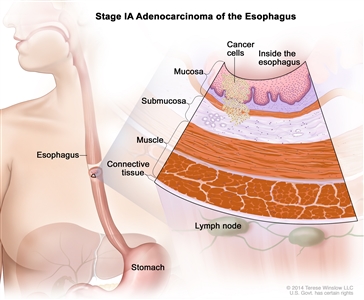
Stage IA adenocarcinoma of the esophagus. Cancer has formed in the mucosa or submucosa layer of the esophagus wall. The cancer cells are grade 1 or 2. Grade 1 and 2 cancer cells look more like normal cells under a microscope and grow and spread more slowly than grade 3 cancer cells. | | N0 = No regional lymph node metastasis. | | M0 = No distant metastasis. | Table 12. Definitions of TNM Stage IB Adenocarcinoma| Stage | Grade | TNMa,b | Description | Illustration |
|---|
| T = primary tumor; N = regional lymph nodes; M = distant metastasis. | | Reprinted with permission from AJCC: Esophageal and esophagogastric junction. In: Edge SB, Byrd DR, Compton CC, et al., eds.: AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer, 2010, pp 103-15. | | The explanations for superscripts a-b are at the end of Table 18. | | IB | 3 | T1, N0, M0 | T1 = Tumor invades lamina propria, muscularis mucosae, or submucosa. |
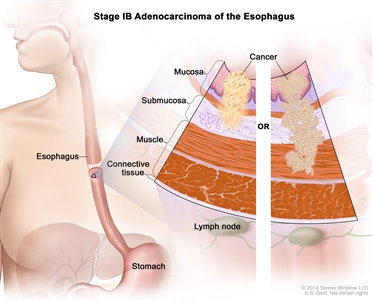
Stage IB adenocarcinoma of the esophagus. Cancer has formed in the mucosa or submucosa layer of the esophagus wall, and the cancer cells are grade 3. Grade 3 cancer cells look more abnormal under a microscope and grow and spread more quickly than grade 1 or 2 cancer cells; OR cancer has formed in the mucosa or submucosa layer and spread into the muscle layer of the esophagus wall, and the cancer cells are grade 1 or 2. Grade 1 and 2 cancer cells look more like normal cells under a microscope and grow and spread more slowly than grade 3 cancer cells. | | N0 = No regional lymph node metastasis. | | M0 = No distant metastasis. | | 1-2, X | T2, N0, M0 | T2 = Tumor invades muscularis propria. | | N0 = No regional lymph node metastasis. | | M0 = No distant metastasis. | Table 13. Definitions of TNM Stage IIA Adenocarcinoma| Stage | Grade | TNMa,b | Description | Illustration |
|---|
| T = primary tumor; N = regional lymph nodes; M = distant metastasis. | | Reprinted with permission from AJCC: Esophageal and esophagogastric junction. In: Edge SB, Byrd DR, Compton CC, et al., eds.: AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer, 2010, pp 103-15. | | The explanations for superscripts a-b are at the end of Table 18. | | IIA | 3 | T2, N0, M0 | T2 = Tumor invades muscularis propria. |
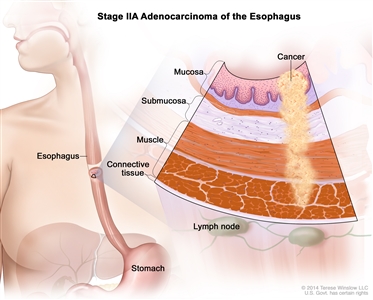
Stage IIA adenocarcinoma of the esophagus. Cancer has spread into the muscle layer of the esophagus wall. The cancer cells are grade 3. Grade 3 cancer cells look more abnormal under a microscope and grow and spread more quickly than grade 1 or 2 cancer cells. | | N0 = No regional lymph node metastasis. | | M0 = No distant metastasis. | Table 14. Definitions of TNM Stage IIB Adenocarcinoma| Stage | Grade | TNMa,b | Description | Illustration |
|---|
| T = primary tumor; N = regional lymph nodes; M = distant metastasis. | | Reprinted with permission from AJCC: Esophageal and esophagogastric junction. In: Edge SB, Byrd DR, Compton CC, et al., eds.: AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer, 2010, pp 103-15. | | The explanations for superscripts a-b are at the end of Table 18. | | IIB | Any | T3, N0, M0 | T3 = Tumor invades adventitia. |
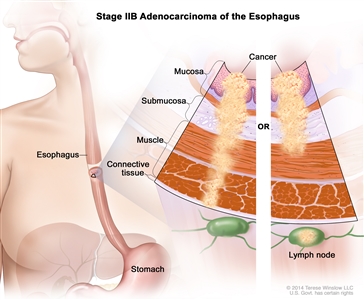
Stage IIB adenocarcinoma of the esophagus. Cancer has spread into the connective tissue layer of the esophagus wall; OR cancer is in the mucosa or submucosa layer and may have spread into the muscle layer of the esophagus wall, and cancer is found in 1 or 2 lymph nodes near the tumor. | | N0 = No regional lymph node metastasis. | | M0 = No distant metastasis. | | Any | T1-2, N1, M0 | T1 = Tumor invades lamina propria, muscularis mucosae, or submucosa. | | T2 = Tumor invades muscularis propria. | | N1 = Metastases in 1-2 regional lymph nodes. | | M0 = No distant metastasis. | Table 15. Definitions of TNM Stage IIIA Adenocarcinoma| Stage | Grade | TNMa,b | Description | Illustration |
|---|
| T = primary tumor; N = regional lymph nodes; M = distant metastasis. | | Reprinted with permission from AJCC: Esophageal and esophagogastric junction. In: Edge SB, Byrd DR, Compton CC, et al., eds.: AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer, 2010, pp 103-15. | | The explanations for superscripts a-b are at the end of Table 18. | | IIIA | Any | T1-2, N2, M0 | T1 = Tumor invades lamina propria, muscularis mucosae, or submucosa. |
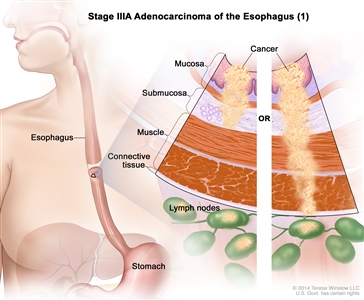
Stage IIIA adenocarcinoma of the esophagus (1). Cancer is in the mucosa or submucosa layer and may have spread into the muscle layer of the esophagus wall, and cancer is found in 3 to 6 lymph nodes near the tumor; OR cancer has spread into the connective tissue layer of the esophagus wall, and cancer is found in 1 or 2 lymph nodes near the tumor.
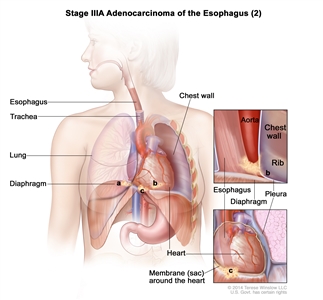
Stage IIIA adenocarcinoma of the esophagus (2). Cancer has spread into the (a) diaphragm, (b) pleura (tissue that covers the lungs and lines the inner wall of the chest cavity), or (c) membrane (sac) around the heart. The cancer can be removed by surgery. | | T2 = Tumor invades muscularis propria. | | N2 = Metastases in 3-6 regional lymph nodes. | | M0 = No distant metastasis. | | Any | T3, N1, M0 | T3 = Tumor invades adventitia. | | N1 = Metastases in 1-2 regional lymph nodes. | | M0 = No distant metastasis. | | Any | T4a, N0, M0 | T4a = Resectable tumor invading pleura, pericardium, or diaphragm. | | N0 = No regional lymph node metastasis. | | M0 = No distant metastasis. | Table 16. Definitions of TNM Stage IIIB Adenocarcinoma| Stage | Grade | TNMa,b | Description | Illustration |
|---|
| T = primary tumor; N = regional lymph nodes; M = distant metastasis. | | Reprinted with permission from AJCC: Esophageal and esophagogastric junction. In: Edge SB, Byrd DR, Compton CC, et al., eds.: AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer, 2010, pp 103-15. | | The explanations for superscripts a-b are at the end of Table 18. | | IIIB | Any | T3, N2, M0 | T3 = Tumor invades adventitia. |
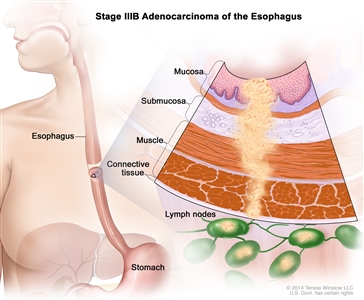
Stage IIIB adenocarcinoma of the esophagus. Cancer has spread into the connective tissue layer of the esophagus wall. Cancer is found in 3 to 6 lymph nodes near the tumor. | | N2 = Metastases in 3-6 regional lymph nodes. | | M0 = No distant metastasis. | Table 17. Definitions of TNM Stage IIIC Adenocarcinoma| Stage | Grade | TNMa,b | Description | Illustration |
|---|
| T = primary tumor; N = regional lymph nodes; M = distant metastasis. | | Reprinted with permission from AJCC: Esophageal and esophagogastric junction. In: Edge SB, Byrd DR, Compton CC, et al., eds.: AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer, 2010, pp 103-15. | | The explanations for superscripts a-c are at the end of Table 18. | | IIIC | Any | T4a, N1-2, M0 | T4a = Resectable tumor invading pleura, pericardium, or diaphragm. |
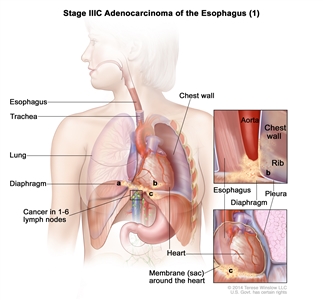
Stage IIIC adenocarcinoma of the esophagus (1). Cancer has spread into the (a) diaphragm, (b) pleura (tissue that covers the lungs and lines the inner wall of the chest cavity), or (c) membrane (sac) around the heart. The cancer can be removed by surgery. Cancer is found in 1 to 6 lymph nodes near the tumor.
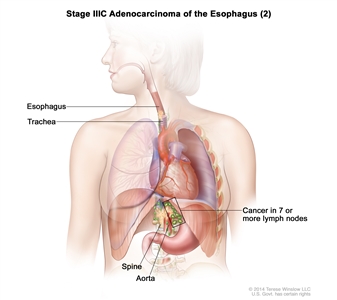
Stage IIIC adenocarcinoma of the esophagus (2). Cancer has spread into nearby organs, such as the aorta, trachea, or spine, and the cancer cannot be removed by surgery; OR cancer has spread to 7 or more lymph nodes near the tumor. | | N1 = Metastases in 1-2 regional lymph nodes. | | N2 = Metastases in 3-6 regional lymph nodes. | | M0 = No distant metastasis. | | Any | T4b, Any N, M0 | T4b = Unresectable tumor invading other adjacent structures, such as aorta, vertebral body, trachea, etc. | | NX = Regional lymph nodes cannot be assessed. | | N0 = No regional lymph node metastasis. | | N1 = Metastases in 1-2 regional lymph nodes. | | N2 = Metastases in 3-6 regional lymph nodes. | | N3 = Metastases in ≥7 regional lymph nodes. | | M0 = No distant metastasis. | | Any | Any T, N3, M0 | TX = Primary tumor cannot be assessed. | | T0 = No evidence of primary tumor. | | Tis = High-grade dysplasia.c | | T1 = Tumor invades lamina propria, muscularis mucosae, or submucosa. | | T1a = Tumor invades lamina propria or muscularis mucosae. | | T1b = Tumor invades submucosa. | | T2 = Tumor invades muscularis propria. | | T3 = Tumor invades adventitia. | | T4 = Tumor invades adjacent structures. | | T4a = Resectable tumor invading pleura, pericardium, or diaphragm. | | T4b = Unresectable tumor invading other adjacent structures, such as aorta, vertebral body, trachea, etc. | | N3 = N3 = Metastases in ≥7 regional lymph nodes. | | M0 = No distant metastasis. | Table 18. Definitions of TNM Stage IV Adenocarcinoma| Stage | Grade | TNMa,b | Description | Illustration |
|---|
| T = primary tumor; N = regional lymph nodes; M = distant metastasis. | | Reprinted with permission from AJCC: Esophageal and esophagogastric junction. In: Edge SB, Byrd DR, Compton CC, et al., eds.: AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer, 2010, pp 103-15. | | a(1) At least maximal dimension of the tumor must be recorded, and (2) multiple tumors require the T(m) suffix. | | b Number must be recorded for total number of regional nodes sampled and total number of reported nodes with metastasis. | | c High-grade dysplasia includes all noninvasive neoplastic epithelia that was formerly called carcinomain situ, a diagnosis that is no longer used for columnar mucosae anywhere in the gastrointestinal tract. | | IV | Any | Any T, Any N, M1 | TX = Primary tumor cannot be assessed. |
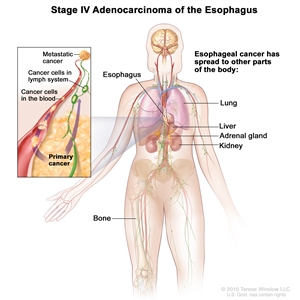
Stage IV adenocarcinoma of the esophagus. The cancer has spread to other parts of the body, such as the lung, liver, adrenal gland, kidney, or bone. | | T0 = No evidence of primary tumor. | | Tis = High-grade dysplasia.c | | T1 = Tumor invades lamina propria, muscularis mucosae, or submucosa. | | T1a = Tumor invades lamina propria or muscularis mucosae. | | T1b = Tumor invades submucosa. | | T2 = Tumor invades muscularis propria. | | T3 = Tumor invades adventitia. | | T4 = Tumor invades adjacent structures. | | T4a = Resectable tumor invading pleura, pericardium, or diaphragm. | | T4b = Unresectable tumor invading other adjacent structures, such as aorta, vertebral body, trachea, etc. | | NX = Regional lymph nodes cannot be assessed. | | N0 = No regional lymph node metastasis. | | N1 = Metastases in 1-2 regional lymph nodes. | | N2 = Metastases in 3-6 regional lymph nodes. | | N3 = Metastases in ≥7 regional lymph nodes. | | M1 = Distant metastasis. | References:
-
Ziegler K, Sanft C, Zeitz M, et al.: Evaluation of endosonography in TN staging of oesophageal cancer. Gut 32 (1): 16-20, 1991.
-
Tio TL, Coene PP, den Hartog Jager FC, et al.: Preoperative TNM classification of esophageal carcinoma by endosonography. Hepatogastroenterology 37 (4): 376-81, 1990.
-
Vazquez-Sequeiros E, Norton ID, Clain JE, et al.: Impact of EUS-guided fine-needle aspiration on lymph node staging in patients with esophageal carcinoma. Gastrointest Endosc 53 (7): 751-7, 2001.
-
Bonavina L, Incarbone R, Lattuada E, et al.: Preoperative laparoscopy in management of patients with carcinoma of the esophagus and of the esophagogastric junction. J Surg Oncol 65 (3): 171-4, 1997.
-
Sugarbaker DJ, Jaklitsch MT, Liptay MJ: Thoracoscopic staging and surgical therapy for esophageal cancer. Chest 107 (6 Suppl): 218S-223S, 1995.
-
Luketich JD, Schauer P, Landreneau R, et al.: Minimally invasive surgical staging is superior to endoscopic ultrasound in detecting lymph node metastases in esophageal cancer. J Thorac Cardiovasc Surg 114 (5): 817-21; discussion 821-3, 1997.
-
Krasna MJ, Reed CE, Nedzwiecki D, et al.: CALGB 9380: a prospective trial of the feasibility of thoracoscopy/laparoscopy in staging esophageal cancer. Ann Thorac Surg 71 (4): 1073-9, 2001.
-
Flamen P, Lerut A, Van Cutsem E, et al.: Utility of positron emission tomography for the staging of patients with potentially operable esophageal carcinoma. J Clin Oncol 18 (18): 3202-10, 2000.
-
Flamen P, Van Cutsem E, Lerut A, et al.: Positron emission tomography for assessment of the response to induction radiochemotherapy in locally advanced oesophageal cancer. Ann Oncol 13 (3): 361-8, 2002.
-
Weber WA, Ott K, Becker K, et al.: Prediction of response to preoperative chemotherapy in adenocarcinomas of the esophagogastric junction by metabolic imaging. J Clin Oncol 19 (12): 3058-65, 2001.
-
van Westreenen HL, Westerterp M, Bossuyt PM, et al.: Systematic review of the staging performance of 18F-fluorodeoxyglucose positron emission tomography in esophageal cancer. J Clin Oncol 22 (18): 3805-12, 2004.
-
Meyers BF, Downey RJ, Decker PA, et al.: The utility of positron emission tomography in staging of potentially operable carcinoma of the thoracic esophagus: results of the American College of Surgeons Oncology Group Z0060 trial. J Thorac Cardiovasc Surg 133 (3): 738-45, 2007.
-
Esophagus and esophagogastric junction. In: Edge SB, Byrd DR, Compton CC, et al., eds.: AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer, 2010, pp 103-11.
-
Korst RJ, Rusch VW, Venkatraman E, et al.: Proposed revision of the staging classification for esophageal cancer. J Thorac Cardiovasc Surg 115 (3): 660-69; discussion 669-70, 1998.
Treatment Option Overview for Esophageal CancerFor patients with minimally invasive resectable esophageal cancer, surgical resection alone offers the potential for cure. In contrast, therapeutic management for patients with locally advanced resectable esophageal cancer has evolved significantly over the last few decades. Because of the risk of distant metastases and local relapse, multimodality therapy with integration of chemotherapy, radiation therapy, and surgical resection has become the standard of care. Combined modality therapies are under clinical evaluation and include the following: - Surgery alone.
- Chemotherapy.
- Radiation therapy.
Effective palliation may be obtained in individual cases with various combinations of the following: - Surgery.
- Chemotherapy.
- Radiation therapy.
- Stents.[1]
- Photodynamic therapy.[2,3,4]
- Endoscopic therapy with Nd:YAG laser.[5]
Table 19. Standard Treatment Options for Esophageal Cancer| Stage ( TNM Staging Criteria) | Treatment Options |
|---|
| Stage 0 Esophageal Cancer | Surgery | | Endoscopic resection | | Stage I Esophageal Cancer | Chemoradiation therapy followed by surgery | | Surgery alone | | Stage II Esophageal Cancer | Chemoradiation followed by surgery | | Surgery alone | | Chemotherapy followed by surgery | | Definitive chemoradiation | | Stage III Esophageal Cancer | Chemoradiation followed by surgery | | Preoperative chemotherapy followed by surgery | | Definitive chemoradiation | | Stage IV Esophageal Cancer | Chemoradiation followed by surgery (for patients with stage IVA disease) | | Chemotherapy, which has provided partial responses for patients with metastatic distal esophageal adenocarcinomas | | Nd:YAG endoluminal tumor destruction or electrocoagulation | | Endoscopic-placed stents to provide palliation of dysphagia | | Radiation therapy with or without intraluminal intubation and dilation | | Intraluminal brachytherapy to provide palliation of dysphagia | | Recurrent Esophageal Cancer | Palliative use of any of the standard therapies, including supportive care | Surgery Surgery (Barrett esophagus) The prevalence of Barrett metaplasia in adenocarcinoma of the esophagus suggests that Barrett esophagus is a premalignant condition. Endoscopic surveillance of patients with Barrett metaplasia may detect adenocarcinoma at an earlier stage that is more amenable to curative resection. Strong consideration should be given to resection in patients with high-grade dysplasia in the setting of Barrett metaplasia.[6] Surgery (esophageal cancer) The survival rate of patients with esophageal cancer is poor. Surgical treatment of resectable esophageal cancers results in 5-year survival rates of 5% to 30%, with higher survival rates in patients with early-stage cancers.[7] Asymptomatic small tumors confined to the esophageal mucosa or submucosa are detected only by chance. Surgery is the treatment of choice for these small tumors. Once symptoms are present (e.g., dysphagia, in most cases), esophageal cancers have usually invaded the muscularis propria or beyond and may have metastasized to lymph nodes or other organs. In some patients with partial esophageal obstruction, dysphagia may be relieved by placement of an expandable metallic stent [8] or by radiation therapy if the patient has disseminated disease or is not a candidate for surgery. Alternative methods of relieving dysphagia have been reported, including laser therapy and electrocoagulation to destroy intraluminal tumor.[9,10,11] In the presence of complete esophageal obstruction without clinical evidence of systemic metastasis, surgical excision of the tumor with mobilization of the stomach to replace the esophagus has been the traditional means of relieving the dysphagia. The optimal surgical approach for radical resection of esophageal cancer is not known. One approach advocates transhiatal esophagectomy with anastomosis of the stomach to the cervical esophagus. A second approach advocates abdominal mobilization of the stomach and transthoracic excision of the esophagus with anastomosis of the stomach to the upper thoracic esophagus or the cervical esophagus. One study concluded that transhiatal esophagectomy was associated with lower morbidity than was transthoracic esophagectomy with extended en bloc lymphadenectomy; however, median overall disease-free and quality-adjusted survival did not differ significantly.[12] Similarly, no differences in long-term quality of life (QOL) using validated QOL instruments have been reported.[13] More recently, minimally invasive approaches that offer potential advantages of smaller incisions, decreased intraoperative blood loss, fewer postoperative complications, and shorter hospital stays have emerged. However, the ability to obtain negative surgical margins, the adequacy of lymph node dissection, and long-term outcomes have not been fully established with this approach.[14] In the United States, the median age of patients who present with esophageal cancer is 67 years.[15] The results of a retrospective review of 505 consecutive patients who were operated on by a single surgical team over 17 years found no difference in the perioperative mortality, median survival, or palliative benefit of esophagectomy on dysphagia when the patients older than 70 years were compared with their younger peers.[16][Levels of evidence: 3iiA and 3iiB] All of the patients in this series were selected for surgery on the basis of potential operative risk. Age alone does not determine therapy for patients with potentially resectable disease. Surgical treatment of esophageal cancer is associated with an operative mortality rate of less than 10%.[7] In an attempt to avoid perioperative mortality and to relieve dysphagia, definitive radiation therapy in combination with chemotherapy has been studied. Preoperative Chemoradiation Therapy On the basis of several randomized trial results, chemoradiation followed by surgery is a standard treatment option for patients with stages IB, II, III, and IVA esophageal cancer. Phase III trials have compared preoperative concurrent chemoradiation therapy with surgery alone for patients with esophageal cancer.[17,18,19,20,21,21,22,23][Level of evidence: 1iiA] The benefit of neoadjuvant chemoradiation has been controversial because of contradictory results of early randomized studies.[17,18,19,20] However, the Chemoradiotherapy for Oesophageal Cancer Followed by Surgery Study (CROSS) has definitively demonstrated a survival benefit for preoperative chemoradiation compared with surgery alone in locally advanced esophageal cancer.[21] For early-stage tumors, the role of preoperative chemoradiation remains controversial. Although the CROSS study included early-stage patients, the Francophone de Cancérologie Digestive (FFCD) 9901 study (NCT00047112)[23], which included only early-stage (stage I or II) patients, failed to demonstrate a survival advantage in this group of patients. Evidence (preoperative chemoradiation therapy): - The CROSS study randomly assigned 366 patients with resectable esophageal or junctional cancers to receive either surgery alone or weekly administration of carboplatin (dose titrated to achieve an AUC [area under the curve] of 2 mg/mL/minute) and paclitaxel (50 mg/m2 of BSA [body surface area]) and concurrent radiation therapy (41.4 Gy in 23 fractions) administered over 5 weeks. Most patients enrolled in the CROSS trial (75%) had adenocarcinoma.[21,24][Level of evidence: 1iiA]
- With a median follow-up of 84 months, preoperative chemoradiation was found to improve median overall survival (OS) from 24 months in the surgery-alone group to 48.6 months (hazard ratio [HR], 0.68; 95% confidence interval [CI], 0.53-0.88; P = .003). Median OS for patients with squamous cell carcinomas was 81.6 months in the preoperative chemoradiation group compared with 21.1 months in the surgery-alone group (HR, 0.48; 95% CI, 0.28-0.83; log rank P = .008); for patients with adenocarcinomas, median OS was 43.2 months in the preoperative chemoradiation group compared with 27.1 months in the surgery-alone group (HR, 0.73; 95% CI, 0.55-0.98; log rank P = .038).[24]
- Additionally, preoperative chemoradiation improved the rate of R0 resections (92% vs. 69%, P < .001). R0 is defined as complete resection with no tumor within 1 mm of resection margins.
- A complete pathologic response was achieved in 29% of patients who underwent resection after chemoradiation therapy. A pathologic complete response was observed in 23% of patients with adenocarcinoma compared with 49% of patients with squamous cell carcinoma (P = .008).
- Postoperative complications and in-hospital mortality were equivalent in both groups. The most common hematologic side effects in the chemoradiation group were leukopenia (6%) and neutropenia (2%). The most common nonhematologic side effects were anorexia (5%) and fatigue (3%).
- With a median follow-up of 84 months, the 5-year progression-free survival (PFS) was 44% in the preoperative chemoradiation group compared with 27% in the surgery-alone group (HR, 0.61 [0.47-0.78]). Preoperative chemoradiation therapy reduced locoregional recurrence from 34% to 14% (P < .001) and peritoneal carcinomatosis from 14% to 4% (P < .001). There was a small but significant effect on hematogenous dissemination in favor of the chemoradiation therapy group (35% vs. 29%; P = .025).[22,24][Level of evidence: 1iiDii]
- A multicenter prospective randomized trial compared preoperative combined chemotherapy (i.e., cisplatin) and radiation therapy (37 Gy in 3.7 Gy fractions) versus surgery alone in patients with squamous cell carcinoma.[17][Level of evidence: 1iiA]
- The study showed no improvement in OS and a significantly higher postoperative mortality (12% vs. 4%) in the combined-modality arm.
- In patients with adenocarcinoma of the esophagus, a single-institution phase III trial was conducted in patients treated with induction chemoradiation therapy consisting of 5-fluorouracil (5-FU), cisplatin, and 40 Gy (2.67 Gy fractions) plus surgery compared with resection alone.[18][Level of evidence: 1iiA]
- The results demonstrated a modest survival benefit of 16 months for combined modality therapy versus 11 months for surgery alone.
- A subsequent single-institution trial randomly assigned patients (75% with adenocarcinoma) to 5-FU, cisplatin, vinblastine, and radiation therapy (1.5 Gy twice daily to a total of 45 Gy) plus resection versus esophagectomy alone.[19][Level of evidence: 1iiA]
- At a median follow-up of more than 8 years, there was no significant difference between the surgery alone and combined modality therapy with respect to median survival (17.6 months vs. 16.9 months), OS (16% vs. 30% at 3 years), or disease-free survival (16% vs. 28% at 3 years).
- An intergroup trial (CALGB-9781) planned to randomly assign 475 patients with resectable squamous cell or adenocarcinoma of the thoracic esophagus to treatment with preoperative chemoradiation therapy (5-FU, cisplatin, and 50.4 Gy) followed by esophagectomy and nodal dissection or surgery alone. The trial was closed as a result of poor patient accrual; however, results from the 56 enrolled patients, with a median follow-up of 6 years, were reported.[20][Level of evidence: 1iiA]
- The median survival was 4.48 years (95% CI, 2.4 years to not estimable) for trimodality therapy versus 1.79 years (95% CI, 1.41-2.59 years) for surgery alone (P = .002), with 5-year OS of 39% for trimodality therapy (95% CI, 21%-57%) versus 16% for surgery alone (95% CI, 5%-33%).
- To further evaluate the impact of neoadjuvant chemoradiation therapy for early-stage disease, FFCD 9901 randomly assigned 195 patients with stage I or stage II esophageal cancer to receive surgery alone or neoadjuvant chemoradiation therapy (45 Gy in 25 fractions administered with two courses of 5-FU [800 mg/m2] and cisplatin [75 mg/m2]) followed by surgery.[23][Level of evidence: 1iiA]
- At interim analysis, accrual to the study was stopped early because of futility.
- With a median follow-up of 94 months, there was no significant improvement in 3-year OS with chemoradiation (48% vs. 53%, P = .94); there was a significantly higher postoperative mortality rate of 11.1% versus 3.4% (P = .049).
Preoperative Chemotherapy The effects of preoperative chemotherapy are being evaluated in randomized trials. Several studies have demonstrated a survival benefit with preoperative chemotherapy compared with surgery alone.[25,26,27] However, one large randomized study failed to confirm a survival benefit with preoperative chemotherapy.[28] Compared with preoperative chemotherapy alone, preoperative chemoradiation therapy improves pathologic response and may improve outcomes.[29] Evidence (preoperative chemotherapy): - An intergroup trial (NCT00525785) randomly assigned 440 patients with local and operable esophageal cancer of any cell type to three cycles of preoperative 5-FU and cisplatin followed by surgery and two additional cycles of chemotherapy versus surgery alone.[28][Level of evidence: 1iiA]
- After a median follow-up of 55 months, there were no significant differences between the chemotherapy plus surgery (14.9 months) and surgery-alone (16.1 months) groups in median survival (35%) or 2-year survival (37%).
- The addition of chemotherapy did not increase the morbidity associated with surgery.
- The Medical Research Council Oesophageal Cancer Working Party randomly assigned 802 patients with resectable esophageal cancer, also of any cell type, to two cycles of preoperative 5-FU and cisplatin followed by surgery versus surgery alone.[25][Level of evidence: 1iiA]
- At a median follow-up of 37 months, median survival was significantly improved in the preoperative chemotherapy arm (16.8 months vs. 13.3 months with surgery alone; difference, 3.5 months; 95% CI, 1.0-6.5 months), as was 2-year OS (43% in the preoperative chemotherapy arm and 34% in the surgery-alone arm; difference, 9%; 95% CI, 3-14 months).
The interpretation of the results from the intergroup and preoperative chemotherapy trials is challenging because T or N staging was not reported, and prerandomization and radiation could be offered at the discretion of the treating oncologist. - The Japanese Clinical Oncology Group randomly assigned 330 patients with clinical stage II or III, excluding T4, squamous cell carcinomas to receive either two cycles of preoperative cisplatin and 5-FU followed by surgery or surgery followed by postoperative chemotherapy of the same regimen. A planned interim analysis was conducted after patient accrual; although the primary endpoint of PFS was not met, there was a significant benefit in OS among patients treated with preoperative chemotherapy (P = .01). As a result of these findings, the Data and Safety Monitoring Committee recommended early closure of the study.[26][Level of evidence: 1iiC]
- With a median follow-up of 61 months, the 5-year OS was 55% among patients treated with preoperative chemotherapy compared with 43% among patients treated with postoperative chemotherapy (P = .04). However, there was no significant difference between groups with respect to PFS (5-year PFS, 39% vs. 44%; P = .22).
- Additionally, there were no significant differences between the two groups with respect to postoperative complications or treatment-related toxicities.
- The Fédération Nationale des Centres de Lutte contre le Cancer (FNCLCC) and the Fédération Francophone de Cancérologie Digestive (FFCD) randomly assigned 224 patients with resectable adenocarcinoma of the lower esophagus, gastroesophageal junction, or stomach to receive either perioperative chemotherapy and surgery (n = 113) or surgery alone (n = 111). Chemotherapy consisted of two or three preoperative cycles of intravenous (IV) cisplatin (100 mg/m2) on day 1 and continuous IV infusion of 5-FU (800 mg/m2) for 5 consecutive days (day 1-5) every 28 days, and three or four postoperative cycles of the same regimen.[27][Level of evidence: 1iiA]
- Perioperative chemotherapy was associated with improved 5-year OS (5-year OS, 38% vs. 24%; HR, 0.69; P = .02).
- Grade 3 and 4 toxicity occurred in 38% of patients treated with perioperative chemotherapy, but there was no increase in postoperative morbidity.
- The Preoperative Chemotherapy or Radiochemotherapy in Esophago-gastric Adenocarcinoma Trial (POET) sought to evaluate the additional benefit of radiation therapy to preoperative chemotherapy. Patients were randomly assigned to receive either induction chemotherapy (15 weeks) followed by surgery or chemotherapy (12 weeks) followed by chemoradiation therapy (3 weeks) followed by surgery.[29][Level of evidence: 1iiA]
- The study was closed early because of poor accrual. In total, 126 patients were randomly assigned.
- Preoperative radiation therapy yielded 3-year survival of 27% to 47% (log rank, P = .07). Postoperative mortality was nonsignificantly increased in the chemoradiation therapy group (10.2% vs. 3.8%, P = .26).
Definitive Chemoradiation For patients who are deemed either medically inoperable or have tumors that are unresectable, the efficacy of definitive chemoradiation has been established in numerous randomized controlled trials.[30,31] For patients with squamous cell carcinomas of the esophagus, definitive chemoradiation may offer equivalent outcomes compared with preoperative chemoradiation followed by surgical resection.[32,33] Evidence (definitive chemoradiation): - A Radiation Therapy Oncology Group trial (RTOG-8501) randomly assigned patients to chemotherapy and radiation therapy versus radiation therapy alone. Patients were randomly assigned to receive radiation therapy alone (64 Gy in 32 fractions) or chemoradiation (50 Gy in 25 fractions) with concurrent cisplatin (75 mg/m2) and continuous-infusion 5-FU (1,000 mg/m2 on days 1 to 4 in weeks 1 and 5 followed by two additional cycles of chemotherapy administered 3 weeks apart).[30][Level of evidence: 1iiA]
- There was an improvement in 5-year survival for the combined modality group (27% vs. 0%).
- An 8-year follow-up of this trial demonstrated an OS rate of 22% for patients receiving chemoradiation therapy.
- Intergroup-0123 (RTOG-9405 ) was conducted in an attempt to improve upon the results of RTOG-8501. Intergroup-0123 randomly assigned 236 patients with localized esophageal tumors to undergo chemoradiation with high-dose radiation therapy (64.8 Gy) and four monthly cycles of 5-FU and cisplatin versus conventional-dose radiation therapy (50.4 Gy) and the same chemotherapy schedule.[31][Level of evidence: 1iiA]
- Although originally designed to accrue 298 patients, this trial was closed in 1999 after a planned interim analysis showed that it was statistically unlikely that there would be any advantage to using high-dose radiation.
- At a 2-year median follow-up, no statistically significant differences in median survival were observed between the high-dose and conventional-dose radiation therapy arms (13 months vs. 18 months), 2-year survival (31% vs. 40%), or local and regional failures (56% vs. 52%).
- There was a higher treatment mortality in the higher-dose arm (9% vs. 2%); however, 7 of 11 deaths in the high-dose arm occurred in patients who had received 50.4 Gy or less.
- An Eastern Cooperative Oncology Group trial (EST-1282) evaluated 135 patients.[34][Level of evidence: 1iiA]
- This trial showed that chemotherapy plus radiation provided a better 2-year survival rate than did radiation therapy alone, similar to results from the intergroup trial.
- The PRODIGE5/ACCORD17 (NCT00861094) trial sought to evaluate and compare the efficacy and safety of FOLFOX (oxaliplatin, fluorouracil, and leucovorin calcium) versus 5-FU and cisplatin as the chemotherapy backbone among patients treated with definitive chemoradiation for localized esophageal cancer. In this multicenter randomized phase II and III trial, 267 patients were randomly assigned to receive either six cycles of FOLFOX (three cycles concomitant with radiation therapy), oxaliplatin (85 mg/m2), leucovorin (200 mg/m2), bolus 5-FU (400 mg/m2) and infusion 5-FU (1,600 mg/m2 over 46 hours) or four cycles of 5-FU (1,000 mg/m2 for 4 days) and cisplatin (75 mg/m2 on day 1). All patients received radiation therapy (50 Gy in 25 fractions).[35][Level of evidence: 1iiDiii]
- With a median follow-up of 25.3 months, there was no significant difference in PFS (9.7 months with FOLFOX vs. 9.4 months with 5-FU and cisplatin; P = .64).
- There was one death caused by toxicity in the FOLFOX group versus six deaths in the 5-FU and cisplatin arm (P = .066).
- There were no significant differences in grade 3 or 4 adverse events between treatment groups. Among toxicities of all grades, paresthesia, sensory neuropathy, and increases in aspartate transaminase and alanine transaminase were more common in the FOLFOX group; whereas, increases in serum creatinine, mucositis, and alopecia were more common in the 5-FU and cisplatin group.
- A phase III German trial also compared induction chemotherapy (three courses of bolus 5-FU, leucovorin, etoposide, and cisplatin) followed by chemoradiation therapy (cisplatin, etoposide, and 40 Gy) followed by surgery (arm A), or the same induction chemotherapy followed by chemoradiation therapy (at least 65 Gy) without surgery (arm B) for patients with T3 or T4 squamous cell carcinoma of the esophagus. OS was the primary outcome.[32][Level of evidence: 1iiA]
- The analysis of 172 eligible, randomly assigned patients showed that OS at 2 years was not statistically significantly different between the two treatment groups (arm A, 39.9%; 95% CI, 29.4%-50.4%; arm B, 35.4%; 95% CI, 25.2%-45.6%; log-rank test for equivalence with 0.15, P < .007).
- Local PFS was higher in the surgery group (2-year PFS, 64.3%; 95% CI, 52.1%-76.5%) than in the chemoradiation therapy group (2-year PFS, 40.7%; 95% CI, 28.9%-52.5%; HR for arm B vs. arm A, 2.1; 95% CI, 1.3-3.5; P < .003).
- Treatment-related mortality was higher in the surgery group (12.8%) than in the chemoradiation therapy group (3.5%) (P < .03).
- FFCD 9102 (NCT00416858) randomly assigned 259 patients with T3N0-1M0 thoracic esophageal cancer to receive either two cycles of 5-FU and cisplatin (days 1-5 and 22-26) and either conventional radiation (46 Gy in 4.5 weeks) or split course (15 Gy, days 1-5 and 22-26). Patients with response were then randomly assigned to receive either surgical resection (arm A) or continuation of chemoradiation (arm B: three cycles of 5FU plus cisplatin and either conventional 20 Gy or split-course 15 Gy radiation therapy).[33][Level of evidence: 1iiA]
- Of the 259 randomly assigned patients, 230 (89%) had squamous cell carcinoma, and 29 patients (11%) had adenocarcinomas.
- The 2-year OS was 34% in patients randomly assigned to receive surgery versus 40% in patients randomly assigned to receive definitive chemoradiation (HR, 0.90; P = .44). Median survival was 17.7 months for surgery and 19.3 months for definitive chemoradiation.
- The 3-month mortality rate was 9.3% in the surgery arm compared with 0.8% in the chemoradiation arm (P = .002).
Postoperative Radiation Therapy Two randomized trials have shown no significant OS benefit for postoperative radiation therapy compared with surgery alone.[36,37][Level of evidence: 1iiA] All newly diagnosed patients should be considered candidates for therapies and clinical trials comparing various treatment modalities. Information about ongoing clinical trials is available from the NCI website. References:
-
Tietjen TG, Pasricha PJ, Kalloo AN: Management of malignant esophageal stricture with esophageal dilation and esophageal stents. Gastrointest Endosc Clin N Am 4 (4): 851-62, 1994.
-
Lightdale CJ, Heier SK, Marcon NE, et al.: Photodynamic therapy with porfimer sodium versus thermal ablation therapy with Nd:YAG laser for palliation of esophageal cancer: a multicenter randomized trial. Gastrointest Endosc 42 (6): 507-12, 1995.
-
Kubba AK: Role of photodynamic therapy in the management of gastrointestinal cancer. Digestion 60 (1): 1-10, 1999 Jan-Feb.
-
Heier SK, Heier LM: Tissue sensitizers. Gastrointest Endosc Clin N Am 4 (2): 327-52, 1994.
-
Bourke MJ, Hope RL, Chu G, et al.: Laser palliation of inoperable malignant dysphagia: initial and at death. Gastrointest Endosc 43 (1): 29-32, 1996.
-
Lerut T, Coosemans W, Van Raemdonck D, et al.: Surgical treatment of Barrett's carcinoma. Correlations between morphologic findings and prognosis. J Thorac Cardiovasc Surg 107 (4): 1059-65; discussion 1065-6, 1994.
-
Kelsen DP, Bains M, Burt M: Neoadjuvant chemotherapy and surgery of cancer of the esophagus. Semin Surg Oncol 6 (5): 268-73, 1990.
-
Saxon RR, Morrison KE, Lakin PC, et al.: Malignant esophageal obstruction and esophagorespiratory fistula: palliation with a polyethylene-covered Z-stent. Radiology 202 (2): 349-54, 1997.
-
Campbell WR Jr, Taylor SA, Pierce GE, et al.: Therapeutic alternatives in patients with esophageal cancer. Am J Surg 150 (6): 665-8, 1985.
-
Mellow MH, Pinkas H: Endoscopic therapy for esophageal carcinoma with Nd:YAG laser: prospective evaluation of efficacy, complications, and survival. Gastrointest Endosc 30 (6): 334-9, 1984.
-
Karlin DA, Fisher RS, Krevsky B: Prolonged survival and effective palliation in patients with squamous cell carcinoma of the esophagus following endoscopic laser therapy. Cancer 59 (11): 1969-72, 1987.
-
Hulscher JB, van Sandick JW, de Boer AG, et al.: Extended transthoracic resection compared with limited transhiatal resection for adenocarcinoma of the esophagus. N Engl J Med 347 (21): 1662-9, 2002.
-
de Boer AG, van Lanschot JJ, van Sandick JW, et al.: Quality of life after transhiatal compared with extended transthoracic resection for adenocarcinoma of the esophagus. J Clin Oncol 22 (20): 4202-8, 2004.
-
Santillan AA, Farma JM, Meredith KL, et al.: Minimally invasive surgery for esophageal cancer. J Natl Compr Canc Netw 6 (9): 879-84, 2008.
-
Ginsberg RJ: Cancer treatment in the elderly. J Am Coll Surg 187 (4): 427-8, 1998.
-
Ellis FH Jr, Williamson WA, Heatley GJ: Cancer of the esophagus and cardia: does age influence treatment selection and surgical outcomes? J Am Coll Surg 187 (4): 345-51, 1998.
-
Bosset JF, Gignoux M, Triboulet JP, et al.: Chemoradiotherapy followed by surgery compared with surgery alone in squamous-cell cancer of the esophagus. N Engl J Med 337 (3): 161-7, 1997.
-
Walsh TN, Noonan N, Hollywood D, et al.: A comparison of multimodal therapy and surgery for esophageal adenocarcinoma. N Engl J Med 335 (7): 462-7, 1996.
-
Urba SG, Orringer MB, Turrisi A, et al.: Randomized trial of preoperative chemoradiation versus surgery alone in patients with locoregional esophageal carcinoma. J Clin Oncol 19 (2): 305-13, 2001.
-
Tepper J, Krasna MJ, Niedzwiecki D, et al.: Phase III trial of trimodality therapy with cisplatin, fluorouracil, radiotherapy, and surgery compared with surgery alone for esophageal cancer: CALGB 9781. J Clin Oncol 26 (7): 1086-92, 2008.
-
van Hagen P, Hulshof MC, van Lanschot JJ, et al.: Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med 366 (22): 2074-84, 2012.
-
Oppedijk V, van der Gaast A, van Lanschot JJ, et al.: Patterns of recurrence after surgery alone versus preoperative chemoradiotherapy and surgery in the CROSS trials. J Clin Oncol 32 (5): 385-91, 2014.
-
Mariette C, Dahan L, Mornex F, et al.: Surgery alone versus chemoradiotherapy followed by surgery for stage I and II esophageal cancer: final analysis of randomized controlled phase III trial FFCD 9901. J Clin Oncol 32 (23): 2416-22, 2014.
-
Shapiro J, van Lanschot JJ, Hulshof MC, et al.: Neoadjuvant chemoradiotherapy plus surgery versus surgery alone for oesophageal or junctional cancer (CROSS): long-term results of a randomised controlled trial. Lancet Oncol 16 (9): 1090-8, 2015.
-
Medical Research Council Oesophageal Cancer Working Group: Surgical resection with or without preoperative chemotherapy in oesophageal cancer: a randomised controlled trial. Lancet 359 (9319): 1727-33, 2002.
-
Ando N, Kato H, Igaki H, et al.: A randomized trial comparing postoperative adjuvant chemotherapy with cisplatin and 5-fluorouracil versus preoperative chemotherapy for localized advanced squamous cell carcinoma of the thoracic esophagus (JCOG9907). Ann Surg Oncol 19 (1): 68-74, 2012.
-
Ychou M, Boige V, Pignon JP, et al.: Perioperative chemotherapy compared with surgery alone for resectable gastroesophageal adenocarcinoma: an FNCLCC and FFCD multicenter phase III trial. J Clin Oncol 29 (13): 1715-21, 2011.
-
Kelsen DP, Ginsberg R, Pajak TF, et al.: Chemotherapy followed by surgery compared with surgery alone for localized esophageal cancer. N Engl J Med 339 (27): 1979-84, 1998.
-
Stahl M, Walz MK, Stuschke M, et al.: Phase III comparison of preoperative chemotherapy compared with chemoradiotherapy in patients with locally advanced adenocarcinoma of the esophagogastric junction. J Clin Oncol 27 (6): 851-6, 2009.
-
Cooper JS, Guo MD, Herskovic A, et al.: Chemoradiotherapy of locally advanced esophageal cancer: long-term follow-up of a prospective randomized trial (RTOG 85-01). Radiation Therapy Oncology Group. JAMA 281 (17): 1623-7, 1999.
-
Minsky BD, Pajak TF, Ginsberg RJ, et al.: INT 0123 (Radiation Therapy Oncology Group 94-05) phase III trial of combined-modality therapy for esophageal cancer: high-dose versus standard-dose radiation therapy. J Clin Oncol 20 (5): 1167-74, 2002.
-
Stahl M, Stuschke M, Lehmann N, et al.: Chemoradiation with and without surgery in patients with locally advanced squamous cell carcinoma of the esophagus. J Clin Oncol 23 (10): 2310-7, 2005.
-
Bedenne L, Michel P, Bouché O, et al.: Chemoradiation followed by surgery compared with chemoradiation alone in squamous cancer of the esophagus: FFCD 9102. J Clin Oncol 25 (10): 1160-8, 2007.
-
Smith TJ, Ryan LM, Douglass HO Jr, et al.: Combined chemoradiotherapy vs. radiotherapy alone for early stage squamous cell carcinoma of the esophagus: a study of the Eastern Cooperative Oncology Group. Int J Radiat Oncol Biol Phys 42 (2): 269-76, 1998.
-
Conroy T, Galais MP, Raoul JL, et al.: Definitive chemoradiotherapy with FOLFOX versus fluorouracil and cisplatin in patients with oesophageal cancer (PRODIGE5/ACCORD17): final results of a randomised, phase 2/3 trial. Lancet Oncol 15 (3): 305-14, 2014.
-
Ténière P, Hay JM, Fingerhut A, et al.: Postoperative radiation therapy does not increase survival after curative resection for squamous cell carcinoma of the middle and lower esophagus as shown by a multicenter controlled trial. French University Association for Surgical Research. Surg Gynecol Obstet 173 (2): 123-30, 1991.
-
Fok M, Sham JS, Choy D, et al.: Postoperative radiotherapy for carcinoma of the esophagus: a prospective, randomized controlled study. Surgery 113 (2): 138-47, 1993.
Stage 0 Esophageal CancerStandard Treatment Options for Stage 0 Esophageal Cancer Stage 0 squamous cell esophageal cancer is rarely seen in the United States, but surgery has been used.[1,2] For early-stage minimally invasive esophageal cancer, surgical and endoscopic techniques offer high rates of cure.[3,4] - Surgery.
- Endoscopic resection.
Current Clinical Trials Check the list of NCI-supported cancer clinical trials that are now accepting patients with stage 0 esophageal cancer. The list of clinical trials can be further narrowed by location, drug, intervention, and other criteria. General information about clinical trials is also available from the NCI website. References:
-
Rusch VW, Levine DS, Haggitt R, et al.: The management of high grade dysplasia and early cancer in Barrett's esophagus. A multidisciplinary problem. Cancer 74 (4): 1225-9, 1994.
-
Heitmiller RF, Redmond M, Hamilton SR: Barrett's esophagus with high-grade dysplasia. An indication for prophylactic esophagectomy. Ann Surg 224 (1): 66-71, 1996.
-
Pech O, Bollschweiler E, Manner H, et al.: Comparison between endoscopic and surgical resection of mucosal esophageal adenocarcinoma in Barrett's esophagus at two high-volume centers. Ann Surg 254 (1): 67-72, 2011.
-
Prasad GA, Wu TT, Wigle DA, et al.: Endoscopic and surgical treatment of mucosal (T1a) esophageal adenocarcinoma in Barrett's esophagus. Gastroenterology 137 (3): 815-23, 2009.
Stage I Esophageal CancerStandard Treatment Options for Stage I Esophageal Cancer Standard treatment options for stage I esophageal cancer include the following:[1,2,3,4,5] - Chemoradiation followed by surgery.
- Surgery alone.
Current Clinical Trials Check the list of NCI-supported cancer clinical trials that are now accepting patients with stage I esophageal cancer. The list of clinical trials can be further narrowed by location, drug, intervention, and other criteria. General information about clinical trials is also available from the NCI website. References:
-
Bosset JF, Gignoux M, Triboulet JP, et al.: Chemoradiotherapy followed by surgery compared with surgery alone in squamous-cell cancer of the esophagus. N Engl J Med 337 (3): 161-7, 1997.
-
Walsh TN, Noonan N, Hollywood D, et al.: A comparison of multimodal therapy and surgery for esophageal adenocarcinoma. N Engl J Med 335 (7): 462-7, 1996.
-
Urba SG, Orringer MB, Turrisi A, et al.: Randomized trial of preoperative chemoradiation versus surgery alone in patients with locoregional esophageal carcinoma. J Clin Oncol 19 (2): 305-13, 2001.
-
Tepper J, Krasna MJ, Niedzwiecki D, et al.: Phase III trial of trimodality therapy with cisplatin, fluorouracil, radiotherapy, and surgery compared with surgery alone for esophageal cancer: CALGB 9781. J Clin Oncol 26 (7): 1086-92, 2008.
-
van Hagen P, Hulshof MC, van Lanschot JJ, et al.: Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med 366 (22): 2074-84, 2012.
Stage II Esophageal CancerStandard Treatment Options for Stage II Esophageal Cancer Standard treatment options for stage II esophageal cancer include the following:[1] - Chemoradiation followed by surgery.[1,2,3]
- Surgery alone.[4,5,6,7]
- Chemotherapy followed by surgery.[8,9,10]
- Definitive chemoradiation.[11,12]
Current Clinical Trials Check the list of NCI-supported cancer clinical trials that are now accepting patients with stage II esophageal cancer. The list of clinical trials can be further narrowed by location, drug, intervention, and other criteria. General information about clinical trials is also available from the NCI website. References:
-
Walsh TN, Noonan N, Hollywood D, et al.: A comparison of multimodal therapy and surgery for esophageal adenocarcinoma. N Engl J Med 335 (7): 462-7, 1996.
-
Tepper J, Krasna MJ, Niedzwiecki D, et al.: Phase III trial of trimodality therapy with cisplatin, fluorouracil, radiotherapy, and surgery compared with surgery alone for esophageal cancer: CALGB 9781. J Clin Oncol 26 (7): 1086-92, 2008.
-
van Hagen P, Hulshof MC, van Lanschot JJ, et al.: Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med 366 (22): 2074-84, 2012.
-
Urba SG, Orringer MB, Turrisi A, et al.: Randomized trial of preoperative chemoradiation versus surgery alone in patients with locoregional esophageal carcinoma. J Clin Oncol 19 (2): 305-13, 2001.
-
Bosset JF, Gignoux M, Triboulet JP, et al.: Chemoradiotherapy followed by surgery compared with surgery alone in squamous-cell cancer of the esophagus. N Engl J Med 337 (3): 161-7, 1997.
-
Conroy T, Galais MP, Raoul JL, et al.: Definitive chemoradiotherapy with FOLFOX versus fluorouracil and cisplatin in patients with oesophageal cancer (PRODIGE5/ACCORD17): final results of a randomised, phase 2/3 trial. Lancet Oncol 15 (3): 305-14, 2014.
-
Mariette C, Dahan L, Mornex F, et al.: Surgery alone versus chemoradiotherapy followed by surgery for stage I and II esophageal cancer: final analysis of randomized controlled phase III trial FFCD 9901. J Clin Oncol 32 (23): 2416-22, 2014.
-
Medical Research Council Oesophageal Cancer Working Group: Surgical resection with or without preoperative chemotherapy in oesophageal cancer: a randomised controlled trial. Lancet 359 (9319): 1727-33, 2002.
-
Ando N, Kato H, Igaki H, et al.: A randomized trial comparing postoperative adjuvant chemotherapy with cisplatin and 5-fluorouracil versus preoperative chemotherapy for localized advanced squamous cell carcinoma of the thoracic esophagus (JCOG9907). Ann Surg Oncol 19 (1): 68-74, 2012.
-
Ychou M, Boige V, Pignon JP, et al.: Perioperative chemotherapy compared with surgery alone for resectable gastroesophageal adenocarcinoma: an FNCLCC and FFCD multicenter phase III trial. J Clin Oncol 29 (13): 1715-21, 2011.
-
Stahl M, Stuschke M, Lehmann N, et al.: Chemoradiation with and without surgery in patients with locally advanced squamous cell carcinoma of the esophagus. J Clin Oncol 23 (10): 2310-7, 2005.
-
Bedenne L, Michel P, Bouché O, et al.: Chemoradiation followed by surgery compared with chemoradiation alone in squamous cancer of the esophagus: FFCD 9102. J Clin Oncol 25 (10): 1160-8, 2007.
Stage III Esophageal CancerStandard Treatment Options for Stage III Esophageal Cancer Standard treatment options for stage III esophageal cancer include the following: - Chemoradiation followed by surgery.[1,2,3]
- Preoperative chemotherapy followed by surgery.[4,5,6]
- Definitive chemoradiation.[7,8,9]
Current Clinical Trials Check the list of NCI-supported cancer clinical trials that are now accepting patients with stage III esophageal cancer. The list of clinical trials can be further narrowed by location, drug, intervention, and other criteria. General information about clinical trials is also available from the NCI website. References:
-
Walsh TN, Noonan N, Hollywood D, et al.: A comparison of multimodal therapy and surgery for esophageal adenocarcinoma. N Engl J Med 335 (7): 462-7, 1996.
-
Tepper J, Krasna MJ, Niedzwiecki D, et al.: Phase III trial of trimodality therapy with cisplatin, fluorouracil, radiotherapy, and surgery compared with surgery alone for esophageal cancer: CALGB 9781. J Clin Oncol 26 (7): 1086-92, 2008.
-
van Hagen P, Hulshof MC, van Lanschot JJ, et al.: Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med 366 (22): 2074-84, 2012.
-
Medical Research Council Oesophageal Cancer Working Group: Surgical resection with or without preoperative chemotherapy in oesophageal cancer: a randomised controlled trial. Lancet 359 (9319): 1727-33, 2002.
-
Ando N, Kato H, Igaki H, et al.: A randomized trial comparing postoperative adjuvant chemotherapy with cisplatin and 5-fluorouracil versus preoperative chemotherapy for localized advanced squamous cell carcinoma of the thoracic esophagus (JCOG9907). Ann Surg Oncol 19 (1): 68-74, 2012.
-
Ychou M, Boige V, Pignon JP, et al.: Perioperative chemotherapy compared with surgery alone for resectable gastroesophageal adenocarcinoma: an FNCLCC and FFCD multicenter phase III trial. J Clin Oncol 29 (13): 1715-21, 2011.
-
Conroy T, Galais MP, Raoul JL, et al.: Definitive chemoradiotherapy with FOLFOX versus fluorouracil and cisplatin in patients with oesophageal cancer (PRODIGE5/ACCORD17): final results of a randomised, phase 2/3 trial. Lancet Oncol 15 (3): 305-14, 2014.
-
Stahl M, Stuschke M, Lehmann N, et al.: Chemoradiation with and without surgery in patients with locally advanced squamous cell carcinoma of the esophagus. J Clin Oncol 23 (10): 2310-7, 2005.
-
Bedenne L, Michel P, Bouché O, et al.: Chemoradiation followed by surgery compared with chemoradiation alone in squamous cancer of the esophagus: FFCD 9102. J Clin Oncol 25 (10): 1160-8, 2007.
Stage IV Esophageal CancerTreatment Options for Stage IV Esophageal Cancer At diagnosis, approximately 50% of patients with esophageal cancer will have metastatic disease and will be candidates for palliative therapy.[1] Treatment options for stage IV esophageal cancer include the following: - Chemoradiation followed by surgery (for patients with stage IVA disease).
- Chemotherapy, which has provided partial responses for patients with metastatic distal esophageal adenocarcinomas.[2,3,4]
- Nd:YAG endoluminal tumor destruction or electrocoagulation.[5]
- Endoscopic-placed stents to provide palliation of dysphagia.[6]
- Radiation therapy with or without intraluminal intubation and dilation.
- Intraluminal brachytherapy to provide palliation of dysphagia.[7,8]
Treatment options under clinical evaluation: Esophageal cancer responds to many anticancer agents. Objective response rates of 30% to 60% and median survivals of less than 1 year are commonly reported with platinum-based combination regimens with 5-FU, taxanes, topoisomerase inhibitors, hydroxyurea, or vinorelbine.[1,4,9] Trastuzumab may be effective in combination with chemotherapy among patients with tumors that overexpress HER2-neu.[10][Level of evidence: 1iiA] - Clinical trials evaluating single-agent or combination chemotherapy.
Current Clinical Trials Check the list of NCI-supported cancer clinical trials that are now accepting patients with stage IV esophageal cancer. The list of clinical trials can be further narrowed by location, drug, intervention, and other criteria. General information about clinical trials is also available from the NCI website. References:
-
Enzinger PC, Ilson DH, Kelsen DP: Chemotherapy in esophageal cancer. Semin Oncol 26 (5 Suppl 15): 12-20, 1999.
-
Waters JS, Norman A, Cunningham D, et al.: Long-term survival after epirubicin, cisplatin and fluorouracil for gastric cancer: results of a randomized trial. Br J Cancer 80 (1-2): 269-72, 1999.
-
Ross P, Nicolson M, Cunningham D, et al.: Prospective randomized trial comparing mitomycin, cisplatin, and protracted venous-infusion fluorouracil (PVI 5-FU) With epirubicin, cisplatin, and PVI 5-FU in advanced esophagogastric cancer. J Clin Oncol 20 (8): 1996-2004, 2002.
-
Taïeb J, Artru P, Baujat B, et al.: Optimisation of 5-fluorouracil (5-FU)/cisplatin combination chemotherapy with a new schedule of hydroxyurea, leucovorin, 5-FU and cisplatin (HLFP regimen) for metastatic oesophageal cancer. Eur J Cancer 38 (5): 661-6, 2002.
-
Bourke MJ, Hope RL, Chu G, et al.: Laser palliation of inoperable malignant dysphagia: initial and at death. Gastrointest Endosc 43 (1): 29-32, 1996.
-
Baron TH: Expandable metal stents for the treatment of cancerous obstruction of the gastrointestinal tract. N Engl J Med 344 (22): 1681-7, 2001.
-
Sur RK, Levin CV, Donde B, et al.: Prospective randomized trial of HDR brachytherapy as a sole modality in palliation of advanced esophageal carcinoma--an International Atomic Energy Agency study. Int J Radiat Oncol Biol Phys 53 (1): 127-33, 2002.
-
Gaspar LE, Nag S, Herskovic A, et al.: American Brachytherapy Society (ABS) consensus guidelines for brachytherapy of esophageal cancer. Clinical Research Committee, American Brachytherapy Society, Philadelphia, PA. Int J Radiat Oncol Biol Phys 38 (1): 127-32, 1997.
-
Conroy T, Etienne PL, Adenis A, et al.: Vinorelbine and cisplatin in metastatic squamous cell carcinoma of the oesophagus: response, toxicity, quality of life and survival. Ann Oncol 13 (5): 721-9, 2002.
-
Bang YJ, Van Cutsem E, Feyereislova A, et al.: Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet 376 (9742): 687-97, 2010.
Recurrent Esophageal CancerPalliation presents difficult problems for all patients with recurrent esophageal cancer. All patients should be considered candidates for clinical trials as outlined in the Treatment Option Overview section of this summary. Standard treatment options: - Palliative use of any of the standard therapies, including supportive care.
Current Clinical Trials Check the list of NCI-supported cancer clinical trials that are now accepting patients with recurrent esophageal cancer. The list of clinical trials can be further narrowed by location, drug, intervention, and other criteria. General information about clinical trials is also available from the NCI website. Changes to This Summary (02 / 02 / 2017)The PDQ cancer information summaries are reviewed regularly and updated as new information becomes available. This section describes the latest changes made to this summary as of the date above. General Information About Esophageal Cancer Updated statistics with estimated new cases and deaths for 2017 (cited American Cancer Society as reference 1). This summary is written and maintained by the PDQ Adult Treatment Editorial Board, which is editorially independent of NCI. The summary reflects an independent review of the literature and does not represent a policy statement of NCI or NIH. More information about summary policies and the role of the PDQ Editorial Boards in maintaining the PDQ summaries can be found on the About This PDQ Summary and PDQ® - NCI's Comprehensive Cancer Database pages. About This PDQ SummaryPurpose of This Summary This PDQ cancer information summary for health professionals provides comprehensive, peer-reviewed, evidence-based information about treatment of esophageal cancer. It is intended as a resource to inform and assist clinicians who care for cancer patients. It does not provide formal guidelines or recommendations for making health care decisions. Reviewers and Updates This summary is reviewed regularly and updated as necessary by the PDQ Adult Treatment Editorial Board, which is editorially independent of the National Cancer Institute (NCI). The summary reflects an independent review of the literature and does not represent a policy statement of NCI or the National Institutes of Health (NIH). Board members review recently published articles each month to determine whether an article should: - be discussed at a meeting,
- be cited with text, or
- replace or update an existing article that is already cited.
Changes to the summaries are made through a consensus process in which Board members evaluate the strength of the evidence in the published articles and determine how the article should be included in the summary. The lead reviewer for Esophageal Cancer Treatment is: - Jennifer Wo, MD (Massachusetts General Hospital)
Any comments or questions about the summary content should be submitted to Cancer.gov through the NCI website's Email Us. Do not contact the individual Board Members with questions or comments about the summaries. Board members will not respond to individual inquiries. Levels of Evidence Some of the reference citations in this summary are accompanied by a level-of-evidence designation. These designations are intended to help readers assess the strength of the evidence supporting the use of specific interventions or approaches. The PDQ Adult Treatment Editorial Board uses a formal evidence ranking system in developing its level-of-evidence designations. Permission to Use This Summary PDQ is a registered trademark. Although the content of PDQ documents can be used freely as text, it cannot be identified as an NCI PDQ cancer information summary unless it is presented in its entirety and is regularly updated. However, an author would be permitted to write a sentence such as "NCI's PDQ cancer information summary about breast cancer prevention states the risks succinctly: [include excerpt from the summary]." The preferred citation for this PDQ summary is: PDQ® Adult Treatment Editorial Board. PDQ Esophageal Cancer Treatment. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/esophageal/hp/esophageal-treatment-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389338] Images in this summary are used with permission of the author(s), artist, and/or publisher for use within the PDQ summaries only. Permission to use images outside the context of PDQ information must be obtained from the owner(s) and cannot be granted by the National Cancer Institute. Information about using the illustrations in this summary, along with many other cancer-related images, is available in Visuals Online, a collection of over 2,000 scientific images. Disclaimer Based on the strength of the available evidence, treatment options may be described as either "standard" or "under clinical evaluation." These classifications should not be used as a basis for insurance reimbursement determinations. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page. Contact Us More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website's Email Us. Last Revised: 2017-02-02 Last modified on: 8 September 2017
|
|